Risk Factors Low Back Pain Baker 2009 Systematic Review Sleeping Sport Sitting Walking
Original Editor - Phil Lock, Tom Allison, Matt Deakin and Anna Mansfield as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - Matthew Deakin, Thomas Allison, Anna Mansfield, Phil Lock, Wanda van Niekerk, Kim Jackson, Mandeepa Kumawat, Evan Thomas, Admin, Jelle Habay and Vidya Acharya
Introduction [edit | edit source]

The Earth Health Organisation describes adolescence as "young people between the ages of 10 and xix years"[1]. This definition is fartherdivided into early adolescence (10-fourteen years old) to late adolescence (fifteen-19 years old) by the United nations Population Fund [2] . Adolescent back pain has been reported to be as common as that of adult populations [3] [4] [5] and has been attributed to a number of factors such equally gender [half dozen] , age [vii] , sitting for long periods [eight] , working at computers [9] , school seating [10] and psychological factors [11].
Epidemiology [edit | edit source]
There has been a high prevalence of low back pain (LBP) in adolescents demonstrated in a number of epidemiological studies [12] . Estimates of the prevalence of dorsum hurting in children and adolescents vary greatly, ranging from 30%-lxx% [13] [14] . The study by Jeffries et al (2007) found a life time prevalence ranging from iv.seven% to 74.4% for spinal or back pain and 7% to 72% for LBP [7] . These ranges depend on the age of the participants and the methodological differences, in particula,r the definition of dorsum hurting used [iii] .
This level of prevalence raises concerns due to the link between LBP in adolescents and chronic LBP in adulthood[15]. A history of symptoms has been found to exist the strongest predictor of future LBP[sixteen] and an early onset in life linked to chronicity[17] [5]. It has been found that the occurrence of back pain in adolescents increases with age, in particular the years of early teens[7].
Growth and evolution of males and females is remarkably similar up to approximately the age of 10[18]. Higher up the age of 10, as a result of puberty, the growth patterns of males and females deviate considerably[18]. By at least the historic period of eighteen or 19 years, puberty is considered to have ceased[7]. With the potential influence of puberty related growth on the incidence of adolescent back pain [19] it is imperative that the range of pubertal ages are taken into consideration in epidemiological studies[7].
Aetiology [edit | edit source]
Factors associated with back pain in adolescents autumn into four main categories:
- Anthropometry - Acme and Weight/Body mass index
- Lifestyle factors - Physical Action vs Sedentary Action
- Mechanical Load - Heavy Schoolbags
- Psychological, social and behavioural factors[3]
- Participation in sports [xx]
Differential Diagnosis [edit | edit source]
Adolescent back pain predominantly falls into three full general categories: muscular, bone-related, and discogenic [21] [22]
Each with feature features equally displayed in this section:
[edit | edit source]
Most mutual causes of back pain in adolescents, as in adults, are idea to ascend from within the muscles [23]. Muscle-related pain tends to be localised to paraspinal muscles of the thoracic or lumbar area rather than over the spine itself[21]
This type of pain is well-nigh commonly related to overuse, but there may be a history of astute injury.
Other relevent contributing factors include:
- Carrying a heavy rucksack[24][25]
- Incorrect sports equipment (due east.g. improper bicycle seat positioning, lack of cushioned insoles for running)[26]
- Psychosocial distress, depression and feet[27] [28]
[edit | edit source]
Bone-related hurting tends to occur at the centre of the spine and usually exacerbated past extension (backward angle)[21], though this finding is not specific.
Common causes of bone related back pain in adolescents include:
Spondylolysis [edit | edit source]
Spondylolysis describes a unilateral/bilateral defect (separation) in the vertebral pars interarticularis, commonly the lower lumbar vertebrae (particularly L5)[29]
- Spondylolysis usually presents in early adolescence and may initially be asymptomatic, only typically manifests every bit aching low back pain exacerbated by hyperextension of the spine and relieved by residual[xxx].
- Spondylolysis is common in boyish athletes with acute low dorsum pain - accounting for 47% of cases in i orthopaedic series[31].
- The take chances of developing Spondylolysis tends to correlate in athletes whose sport requires repetitive flexion/extension or hyperextension eastward.thou. gymnastics, football, cricket (fast bowlers), weight lifting etc.[26]
Spondylolisthesis [edit | edit source]
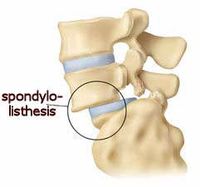
Spondylolithesis - Inductive Vertbral Translation
Spondylolisthesis occurs when bilateral pars defects allow the vertebral body to slip anteriorly. The near common spondylolytic defects occur at the isthmus[32]
- Spondylolysis progresses to spondylolisthesis in approximately 15 % of cases.[33]
- Progression mostly occurs during the teenage growth spurt (with minimal alter later on 16 years)[34] [35].
- Morita et al (1995)[36] suggests spondylolytic progression is correlated with chronicity of pain. However, Seitsalo et al 1991[37] argue that pain frequency has a stronger correlation to kyphotic severity (lumbosacral region).
VIDEO ANIMATION - Click here [X] (Select Spondylolithesis)
Adolescent Idiopathic Scoliosis(AIS) [edit | edit source]
Scoliosis is an abnormal lateral curvature of the spine. Information technology can exist idiopathic (unknown cause) or result from congenital spinal anomalies, muscular spasm or paralysis, infection, tumor, or other causes
- AIS is the most common form of idiopathic scoliosis, bookkeeping for 80 - 85% of cases[38]
- AIS is also noted as the most common spinal deformity seen by primary intendance physicians, pediatricians, and spinal surgeons[39].
- The prevalence of adolescents with a spinal curvature or Cobb angle ≥10º is approximately 3 %.
- AIS has an equal prevalence in males and females,though, the risk of curve progression and therefore the need for later treatment is 10 x higher in females
- Only 1 in x adolescents with idiopathic scoliosis require treatment though[forty]
Scheuermann's Disease / Juvenile Kyphosis [edit | edit source]
- Sheuermann's Disease is the abnormal growth (Osteochondrosis) typically of the thoracolumbar region of the spine leading to increasing spinal curvature
- It may exist associated with spondylosis[41]
- Scheuermann's is the nigh common cause of structural kyphosis in adolescents with a prevalence of 1-viii% and often accompanied with poor posture and backache[42]
[edit | edit source]
Disc-related pain is mostly exacerbated by flexion (forward bending) and may radiate[21]. Approximately 10% of persistent back pain in adolescents is disc related.[43]
Disc Herniation [edit | edit source]
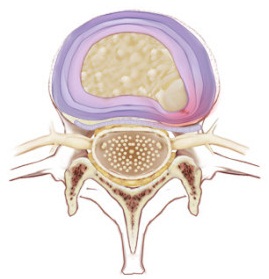
Nucleus pulposus migrating in postero-lateral direction
Disc herniation is a common disorder amid adults with degenerated intervertebral discs with a lifetime occurrence as loftier as twoscore%[44]. However, its occurrence in adolescence is much less frequent at 3-8%[45] as adolescents tend to take a healthier lumbar spine.[46] [47]
Vertebral bodies are separated by intervertebral discs, (to provide back up and mobility). The intervertebral disc is composed of 2 Layers:
- Tough, ligamentous outer annulus
- Gelatinous inner nucleus pulposus.
A combination of intervertebral pressure and degeneration of the ligamentous fibres tin lead to a tear in the annulus - allowing herniation of the nucleus pulposus.
Risk factors for disc herniation include:[13] [48]
- Acute trauma
- Scheuermann'southward disease
- Family history of disc herniation
- Obesity
- Sporting activities e.thou. weight lifting, wrestling, gymnastics, and collision sports
Other possible Causes of Back Pain [edit | edit source]

Osteoid Osteoma - CT Imaging
Tumor [edit | edit source]
- Back pain caused by a spinal tumor is a rare occurrence[49]
- The most mutual tumor that presents with dorsum hurting in adolescents is Osteoid Osteoma [50], a beneficial tumor characterized by nocturnal pain and prompt relief with NSAID'south, although these features are variable.
- Simply ten to 20% of osteoid osteomas are localised to the spine[51]
Infection [edit | edit source]
- Infectious causes of back pain in adolescents include vertebral osteomyelitis, sacroiliac joint infection, epidural abscess, and nonspinal infections (eg, paraspinous muscle abscess, endocarditis, and myalgia (muscle pain) associated with viral illness)
Inflammatory Arthritis [edit | edit source]
- A limited number of systemic inflammatory conditions touch the spine and manifest as back hurting
- Weather include ankylosing spondylitis, psoriatic arthritis and reactive arthritis.
- The hallmark of inflammatory affliction is morning stiffness
- Some patients experience aching nocturnal pain that makes it uncomfortable to turn over in bed simply severe dorsum pain is unusual[52]
Differential Diagnosis of Back Pain in Children and Adolescents[53] [edit | edit source]
| Presentation | Possible diagnosis | Associated symptoms |
|---|---|---|
| Night fourth dimension pain | Tumor, infection | Fever, malaise, weight loss |
| Pain with fever or other generalized symptoms | Tumor, infection | Nighttime time pain |
| Astute pain | Herniated deejay, slipped apophysis, spondylolysis Vertebral fracture Musculus strain | Radicular pain, positive straight leg raising test result Other injuries, neurologic loss Muscle tenderness without radiation |
| Chronic hurting | Scheuermann's kyphosis Inflammatory spondyloarthropathies Psychological problems | Rigid kyphosis Morning time stiffness, sacroiliac joint tenderness - |
| Hurting with spinal forward flexion | Herniated disk, slipped apophysis | Radicular pain, positive straight leg raising test result |
| Pain with spinal extension | Spondylolysis, spondylolisthesis, lesion or injury in the pedicle or lamina (posterior arch) | Hamstring tightness |
| Pain with recent-onset scoliosis | Tumor, infection, herniated disk, syrinx Idiopathic scoliosis | Fever, malaise, weight loss, positive straight leg raising test issue Symptoms most mutual in patients xv years and older |
| Other | Pyelonephritis, sickle cell crisis | Aberrant urinalysis findings, dysuria, fever, other bone hurting, history of sickle cell affliction |
Diagnostic Tools and Assessment [edit | edit source]
Past studies have suggested that children with depression dorsum hurting likely suffer from serious spinal pathologies, such equally infections and tumors.[54] [55][56] These studies provided the evidence for the extensive diagnostic workup of pediatric low back pain expert today.
However, recent epidemiological evidence has indicated pediatric low back hurting may be much more prevalent than previously perceived and often mechanical in nature.[57] [58] Equally a result a far greater emphasis is existence placed on conducting a thorough subjective history and physical examination, before performing plush and often inconclusive diagnostic tests.[59] [22]
Subjective History [edit | edit source]
The subjective history should include:[sixty] [61]
| Blazon of Symptoms | What to specifically look for |
|---|---|
| Description of the hurting characteristics | Location, Type, Onset, Elapsing, Change with Activity or Rest, Aggravating and Easing Factors, 24 hour blueprint, Dark Pain |
| Trauma | Acute Macrotrauma, Repetitive Microtrauma, Athletic Activities, Recent/Remote |
| Mechanical symptoms | Worse during or afterward activity |
| Inflammatory symptoms | Morning stiffness, How long? Better with movement? |
| Systemic symptoms | Fever, Dark Sweats, Weight Loss |
| Neurological symptoms | Radiculopathy, Weakness, Bowel or Float Dysfunction |
| Gait | Foot Drop, Aberrant Patterns of Movement |
| Current level of office | Activities, Hobbies, What tin they still practice? |
| Psychosocial factors | Lifestyle, Interference with School, Backpack Weight, Emotional Significance/ Low |
| Previous Injury/Treatment | A history of previous Injury or Surgery, Handling with Immunosuppressive Agents, Scoliosis, Osteoporosis, Malignancy, Neurological disorder, or Chronic Inflammatory Joint Disease |
| Family unit history | Orthopedic, Neurologic, Rheumatic diseases (Ankylosing Spondylitis, Reactive Arthritis, Psoriasis, Inflammatory Bowel Disease). Family History of Back Pain. |
Physical Examination [edit | edit source]
The concrete examination should include:[61][22] [60]
Observations [edit | edit source]
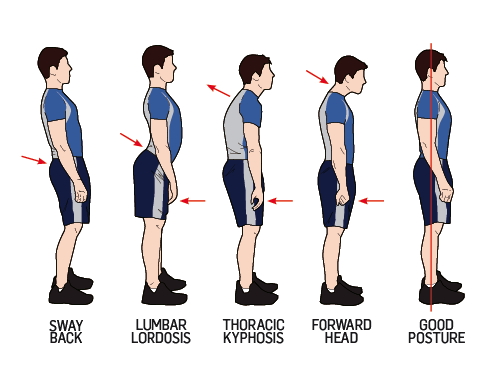
- Posture, pelvis heights, lower limb alignment, foot arches, skin markings are observed with the patient standing
- Lower limb lengths and alignment can be assessed in supine or sitting position
Range of Movement [edit | edit source]
Reproduction of symptoms, quality of movement and resistance should exist observed.
- Agile movements of the spine (flexion = 40°-threescore°, extension = 20°-35°, lateral flexion = 15°-xx°and rotation = 3°-18°) should be tested in a standing position with the pelvis/iliac crest stabilized
- Passive physiological intervertebral movements (PPIVM's) of the spine can exist performed in side lying/ supine/ sitting to assess the range of movement at each segment of the spine
- Passive accessory intervertebral movements (PAIVM's) can be performed in supine/ decumbent as required
Resisted Isometric Movements [edit | edit source]
The following resisted movements should be performed with the spine in a neutral position
- Flexion, extension, lateral flexion and rotation
- Painful movements should be performed last
Provided neutral testing is normal further testing tin be performed:
- Dynamic abdominal endurance
- Dynamic extensor endurance
- Double directly leg lowering
Palpation [edit | edit source]
The point of tenderness should be correlated with the underlying bone or soft tissue anatomy (e.thousand. spinous processes, facet joints, paraspinal muscles, sacroiliac joints, gluteal muscles, posterior superior iliac spines, posterior iliac crest, ischial tuberosities and greater trochanters).
Peripheral Articulation Scanning [edit | edit source]
The following joints should be quickly scanned to rule out any contributing pathology, and whatever deviation from the normal should lead to a more detailed examination of the joint:
- Sacroiliac
- Hip
- Knee
- Ankle
Neurological Test [edit | edit source]
Should the patient history propose potential neurological interest the post-obit tests should be performed:
- Dermatomes
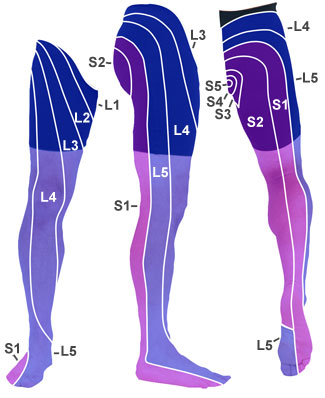
Lower limb dermatomes
- Myotomes
| L2 | Hip Flexion |
| L3 | Knee Extension |
| L4 | Ankle Dorsiflexion |
| L5 | Great Toe Extension |
| S1 | Talocrural joint Plantarflexion/ Eversion |
| S2 | Knee Extension |
- Awareness of the lower leg in major dermatomes
- Deep tendon reflex tests e.one thousand. Patellar (L2, 3, iv), Achilles (S1)
- Pathologic reflexes e.yard. Babinski test
- Hot/Cold, Abrupt/ Blunt
Special Tests [edit | edit source]
Special tests should always be considered an integral function of a much larger examination procedure. [60]
Beneath are some examples of special tests that can assist in the diagnosis of a back hurting patient:
- Slump
- Directly leg raise
- Stork
- Trendelenberg Examination
- Adams Test
- Schober and Modified Schober
- Thomas Test
- OBER
- FABER or Patrick's Test
Red Flags [edit | edit source]
The "red flags" of back pain are important historical and concrete features that point to potentially dangerous conditions. [62] Identification of a ruddy flag in both the subjective history and physical examination warrants close attention and further diagnostic testing.[63]
Spinal "red flags" and their causes include:
| Spinal Reddish Flags | Potential Causes |
| Duration > 6 weeks | Tumor, Infection, Rheumatologic disorders |
| Age < 18 years old | Congenital defect, Tumor, Infection, Spondylolysis, Spondylolysthesis |
| Major trauma | Fracture |
| Cancer | Tumor |
| Fever, Chills, night sweats | Tumor, Infection |
| Weight loss | Tumor, Infection |
| Drug utilize | Infection |
| Night pain | Tumor, Infection |
| Unremitting hurting, fifty-fifty when in supine | Tumor, Infection, Abdominal aortic aneurysm, Nephrolithiasis |
| Pain worsened by coughing, sitting | Herniated disc |
| Pain radiating below knee | Herniated disc, Nerve root compression below L3 nerve root |
| Fecal and urinary incontinence, Sexual dysfunction | Cauda equina syndrome, spinal chord compression |
| Saddle amazement | Cauda equina syndrome, spinal chord compression |
| Severe or speedily progressing neurological deficit | Cauda equina syndrome, spinal chord compression |
Past definition, teenagers with dorsum hurting fulfil i of these red flags as they are under 20 years former, requiring a high alphabetize of suspicion.[64]
- Age <20 years (particularly prepubertal)
- Sudden onset of astringent back pain
- Duration >4 weeks
- Thoracic spine hurting
- Nighttime pain or wakes patient from slumber
- Unremitting hurting, even when supine
- Fever, chills, night sweats
- Unexplained weight loss
- Immunocompromise or HIV
- Previous malignancy
- Corticosteroid use
- Recent trauma
- Progressive neurological deficit
- Float or bowel dysfunction
- Saddle anaesthesia
- Disturbed gait or limp
- Vertebral tenderness or deformity
Yellow Flags [edit | edit source]
In that location take been associations demonstrated between adolescent LBP and diverse psychosocial factors including:[11]
- Depressive symptoms and perceived stress[28]
- Poor wellbeing[65]
- Negative affect[66]
- Hyperactivity[67]
- Emotional and conduct problems[67] [68]
In addition, stressful experiences in childhood have been associated with an increased adventure of chronic LBP (CLBP) in later life[69]. Catastrophizing and a family unit history of chronic pain have both been shown to be associated with a greater level of disability in adolescents with CLBP[lxx].
In summary there is skilful testify that adolescents with LBP are more likely to report negative psychosocial experiences and there is some evidence to support the hypothesis that such negative experiences predict those at high risk of onset[3].
Further Investigations [edit | edit source]
When a thorough subjective history and physical exam are not sufficient to rule out an organic cause of back pain, imaging is performed.[59] [22]
Despite multiple studies examining the diagnostic accuracy of magnetic resonance imaging (MRI), single photon emission computer tomography (SPECT) and plain film radiography in diagnosing specific weather condition (e.1000. spondylolysis, spondylolisthesis, disc herniation),[71] [72] [73] [74] [75] [76] at that place is limited evidence regarding which of these imaging techniques should be used every bit an initial screening tool to evaluate boyish low back hurting.[59]
Imaging [edit | edit source]
Radiographs [edit | edit source]
When clinical findings practise not sufficiently rule out an organic crusade of dorsum pain in children, plain film radiography of the lumbar spine (anteroposterior, lateral and oblique views) is the virtually mutual diagnostic test. [72] [73] [59] [22]

Anteroposterior radiograph of the chest
Bone Browse [edit | edit source]
Os scans help to place areas of increased osteoblast activity and tin can help to localise areas of bone injury not immediately apparent on radiographs.[59] [22]
SPECT(Single Photon Emission Computed Tomography)
Information technology is recommended for imaging the spine in patients who have negative radiographs and no neurological findings. SPECT is especially useful in diagnosing stress fractures and spondylolysis.[71] [73] [75]
Magnetic Resonance Imaging (MRI) [edit | edit source]
MRI allows for increased soft tissue contrast assuasive more detailed evaluation of the spinal cord and surrounding structures. MRI is useful in the diagnosis of back pain with neurological findings (e.g. disc herniation, nerve root compression/ irritation). [74] [76] [22]
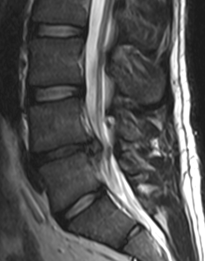
MRI herniated disk
Investigations [edit | edit source]
Laboratory tests are necessary in evaluating patients with back pain and a high suspicion of infection or systemic disease. HLA-B27 and rheumatoid factor are useful in diagnosing inflammatory conditions. Blood and joint cultures should be performed if infection is suspected.[22]
Testify [edit | edit source]
Auerbach et al., (2008)[59] performed a retrospective cohort study on 100 children (mean age = 13.5). All subjects received radiographs, MRI's and SPECT scans. The negative predictive values (NPV) and sensitivity of each test was explored on an individual basis and also in tandem with each other and findings from the physical examination. The results of the study are summarised below:
| Imaging | NPV | Sensitivity |
| Radiograph | 0.68 | 0.38 |
| SPECT | 0.75 | 0.56 |
| MRI | 0.79 | 0.65 |
| Radiography + SPECT + decrease hamstring length | 0.87 | 0.ninety |
| Radiography + MRI + decrease hamstring length | 0.90 | 0.90 |
| Radiography + SPECT + pain on hyperextension | 0.98 | 0.98 |
| Radiography + MRI + hurting on hyperextension | ane | 1 |
In all cases MRI had the highest NPV and sensitivity. It was about effective when combined with a radiograph and pain on hyperextension.
- Withal MRI has a considerably increased cost compared to all other imaging techniques.
- The study found that for subjects with duration of symptoms of < six weeks, SPECT was 100% predictive of mechanical back pain.
- For patients with duration > six weeks MRI was the most effective diagnostic tool but was dependent on the hyperextension test being positive.
Outcome Measures [edit | edit source]
There are many different outcome measures that may exist used by physiotherapists in their treatment of adolescents with back pain.
These include:
- Pain e.yard. visual counterpart scale (VAS), Painometer (a smartphone app to assess pain intensity)
- Disability e.g. Modified Oswestry Disability Questionnaire, Roland & Morris Disability Questionnaire
- Flexibility eg Back-saver sit down and reach
- Endurance e.g. number of sit down ups, squats etc
- Mental health eg Beck Youth Inventories
- Quality of life e.g. Child Wellness Questionnaire Kid Form 87
- Function
- Self efficacy
- Return to sport
- Return to written report/work
Physiotherapy Handling [edit | edit source]
- Treatment of LBP in adults has been investigated extensively[77]. Evidence has shown that physiotherapy handling with practice, backschool and manual therapy are effective in reducing pain and functional limitations in adults [78] [79].
- A report looking at low back pain in adolescent athletes suggested that despite undergoing pubescent changes into adulthood, adolescents cannot be treated like young adults. Therefore, treatment of adolescents can be hard and must be approached differently, with a proficient understanding of spinal development. [80]
- Investigation and practice of therapeutic treatments for children and adolescents with dorsum pain is more contempo than with adults [77]
- Suggested treatments include back education, practice, manual therapy and therapeutic workout.
- These interventions are primarily aimed at decreasing the prevalence, and lessening the intensity of LBP and disability[77]
- Nevertheless, at that place is a dearth of good quality research data in the boyish population[81]
Prevention of LBP [edit | edit source]
- Preventative treatments accept been carried out over the last 3 decades, including concrete therapy exercises, postural hygiene and the promotion of physical activity [77]
- The best prevention of back pain is early detection [82]
- Preventative measures can include 'proper technique' e.one thousand. in lifting sports and limiting excessive lumbar lordosis, plus participating in cadre-strengthening exercises and stretches for tight hamstrings and hip flexors which also may assist reduce the risk of depression back pain[83]
School Backpacks and LBP [edit | edit source]

Some literature suggests that backpacks carried by schoolchildren can cause back pain if they are to heavy or if the weight is carried unevenly.
According to this group-randomised control trial (RCT) the post-obit should be advised to prevent LBP:[84]
- Load the minimum weight possible
- Carry a school backpack on 2 shoulders
- Right the belief that school backpack weight does not affect the dorsum
- Using a locker at schoolhouse
The written report found that children were able to learn salubrious backpack habits. However, this written report was in master schoolhouse aged children rather than secondary, therefore results may non be relevant for an adolescent population.[84]
Interventions [edit | edit source]
It has been ended that physiotherapy treatments are effective in treating adolescents with LBP[77]. A report by Ickmans M et al. provides prove that rehabilitation programs have long-0term effects on people with chronic pain[85]. Some of the suggested treatments are outlined beneath:
Back Education [edit | edit source]
Theoretical or applied educational activity involving:
- Acquisition of knowledge
- Posture training habits
- Body awareness training
Practice [edit | edit source]
- Stretching
- Strengthening
- Breathing
- Posture correction exercises
- Residual exercises
- Functional exercises
- Relaxation
- Coordination
- Stabilisation- stabilisation, or 'core stability', exercises defined every bit: facilitation of deep muscles of the spine (primarily transversus abdominis or multifidus) at depression level, integrated into exercise, progressing into functional activity.[86] [86]
A report which evaluated the efficacy of an practise program for recurrent not-specific dorsum hurting in adolescents, concluding that an practise was an effective short-term handling strategy, incorporated the post-obit forms of exercise[87]:

Knee to chest stretch
- Hurting relieving exerciseswhich encourage motion of the lumbar spine to reduce joint stiffness such as the 'cat stretch' and flexibility exercises for the hip and knee, such every bit knees to breast and knees to the side.
- Reconditioning exercises aiming to provide muscle endurance of lumbar stabilisers and help encourage appropriate motor control of musculus recruitment such as 'superman' single leg extension holds in 4 signal kneeling.
- Progressive exercises imposing a higher challenge on the lumbar stabilisers and more strength related activities, for case horizontal side support on feet.
Manual Therapy [edit | edit source]

Central PA mobilisation to the lumbar spine
- Mobilisation
- Manipulation
- Massage
Meet Manual Therapy Techniques For The Lumbar Spine
Therapeutic Physical Conditioning [edit | edit source]

A teenager enjoying keeping active
This is general fitness and includes any general cardiovascular exercise, for instance[77]:
- Walking
- Running
- Swimming
- Cycling
Evidence [edit | edit source]
- This meta analysis[77], in 2013, examined the differential effectiveness of physiotherapy treatment for LBP in children and adolescents aiming to determine whether the treatments were benign for pain and disability among other effect variables, and which most well-nigh constructive.
- Prior to this analysis, at that place was no solid testify to suggest which treatment was near effective for adolescents with back pain.
- All the handling result measures reached a statistically significant effect magnitude and showed a clinically relevant comeback of symptoms.
- The nearly effective combination treatment was therapeutic physical conditioning (ie full general fitness) and manual therapy.
- However, in that location was express details of what the treatments really involved.
Intensity and Duration of Treatment [edit | edit source]
The study found that the boilerplate:
- Number of weeks of treatment was 12
- Time per week spent engaging in handling was i hr
Quality of the Study [edit | edit source]
The meta-assay itself has good methodological quality, however, at that place was a low number of applicative studies with only 8 articles met the selection criteria. At that place was too a lack of control groups and methodological quality of the studies were poor. This prevents definite conclusions being fatigued. Furthermore, no evidence was provided regarding the duration of the beneficial effects, or details of follow up.
Discussion [edit | edit source]

- There is a demand to incorporate care and do into concrete pedagogy curricula in schools[87] [88] .
- Interestingly, an RCT found that an active physiotherapy programmeimproved adolescent experience of back pain regardless of whether the plan consisted ofsupervised exercises by a physiotherapist[89].
- When treating adolecsents it is important to remember that they are dissimilar to adults, and therefore factors such as growth, age and boredom should be taken into business relationship.
- Treatment of boyish athletes, as well as helping alleviate current symptoms, should address flexibility and musculus imbalance to prevent future injuries[80] [83]
- Render to sport should be a gradual process one time the pain has resolved and the athlete has regained full force[80] [83]
- There is piffling literature regarding the prognosis of back pain in adolescents. Still, an observational study found that adolescents with LBP due to sports participation experienced less improvement in disability than non participants, which may indicate a worse prognosis for sports participants [90]
For more inormation regarding young athletes and LBP click hither.
Conclusion [edit | edit source]
In conclusion, in that location are many suggested physiotherapy treatments for adolescents with dorsum pain. Well-nigh of these are similar to those suggested for adults with back pain. Research suggests a combincation of general fitness excerise and manual therapy are the most effective physiotherapy treatments for adolescents with back hurting.[77] Due to there being a dearth in skillful quality research, in that location is a big demand for more enquiry to exist carried out. Future studies conducted in children and adolescents with LBP should incorporate what has been learnt from adult LBP enquiry and be of rigorous methodological quality[81],.
References [edit | edit source]
- ↑ Who.int. WHO | Adolescent health [Internet]. 2015 [cited 9 January 2015]. Bachelor from: http://www.who.int/topics/adolescent_health/en/
- ↑ Unfpa.org. UNFPA - Un Population Fund | State of Globe Population 2003 [Cyberspace]. 2003 [cited 12 January 2015]. Available from: http://world wide web.unfpa.org/publications/state-world-population-2003
- ↑ three.0 iii.1 3.two 3.three Jones G, Macfarlane G. Epidemiology of low dorsum pain in children and adolescents. Archives of Disease in Childhood. 2005;90(iii):312-316.
- ↑ Burton A, Clarke R, McClune T, Tillotson K. The Natural History of Low Dorsum Pain in Adolescents. Spine. 1996;21(20):2323-2328.
- ↑ 5.0 v.ane Harreby M, Neergaard K, Hesselsôdue east M, Kjer J. Are Radiologic Changes in the Thoracic and Lumbar Spine of Adolescents Run a risk Factors for Depression Back Pain in Adults?. Spine. 1995;20(21):2298-2302.
- ↑ Grimmer K, Nyland L, Milanese S. Longitudinal investigation of low back pain in Australian adolescents: a 5-year written report. Physiother Res Int. 2006;xi(3):161-172.
- ↑ 7.0 7.one 7.two vii.three 7.iv Jeffries L, Milanese S, Grimmer-Somers K. Epidemiology of Adolescent Spinal Pain. Spine. 2007;32(23):2630-2637.
- ↑ Grimmer Thousand, Williams 1000. Gender-age environmental associates of boyish depression back hurting. Applied Ergonomics. 2000;31(4):343-360.
- ↑ Hakala P, Rimpela A, Saarni 50, Salminen J. Frequent computer-related activities increment the risk of neck-shoulder and low back hurting in adolescents. The European Periodical of Public Health. 2005;16(5):536-541.
- ↑ Troussiere B, Tesniere C, Fauconnier J, Grison J, Juvin R, Phelip 10. Comparative report of two different kinds of school article of furniture among children. Ergonomics. 1999;42(iii):516-526.
- ↑ 11.0 11.1 Astfalck R, O'Sullivan P, Straker L, Smith A. A detailed characterisation of pain, disability, physical and psychological features of a small-scale group of adolescents with non-specific chronic low back pain. Manual Therapy. 2010;15(three):240-247.
- ↑ Pellisé F, Balagué F, Rajmil L, Cedraschi C, Aguirre One thousand, Fontecha C et al. Prevalence of Low Back Pain and Its Effect on Wellness-Related Quality of Life in Adolescents. Archives of Pediatrics & Adolescent Medicine. 2009;163(1):65.
- ↑ xiii.0 13.i Balagué F, Troussier B, Salminen J. Non-specific depression back pain in children and adolescents: run a risk factors. European Spine Periodical. 1999;eight(6):429-438.
- ↑ Wedderkopp Northward, Leboeuf-Yde C, Andersen Fifty, Froberg One thousand, Hansen H. Back Hurting Reporting Pattern in a Danish Population-Based Sample of Children and Adolescents. Spine. 2001;26(17):1879-1883.
- ↑ Hestbaek Fifty, Leboeuf-Yde C, Kyvik 1000, Manniche C. The Form of Low Back Pain From Adolescence to Machismo. Spine. 2006;31(4):468-472.
- ↑ Papageorgiou A, Croft P, Thomas E, Ferry S, Jayson M, Silman A. Influence of previous pain feel on the episode incidence of depression back hurting: results from the Southward Manchester Dorsum Pain Study. Pain. 1996;66(2-three):181-185.
- ↑ Brattberg 1000. The incidence of dorsum pain and headache among Swedish school children. Qual Life Res. 1994;3(S1):S27-S31.
- ↑ 18.0 18.ane Brundtland 1000, Liestol K, Walloe L. Meridian and weight of school children and adolescent girls and boys in Oslo 1970. Acta Paediatrica. 1975;64(4):565-573.
- ↑ Feldman D. Risk Factors for the Development of Low Dorsum Hurting in Adolescence. American Periodical of Epidemiology. 2001;154(1):thirty-36.
- ↑ Fritz JM, Clifford SN. Depression back pain in adolescents: a comparison of clinical outcomes in sports participants and nonparticipants. Journal of able-bodied grooming. 2010 Jan;45(1):61-6.
- ↑ 21.0 21.one 21.2 21.3 Metzl J. Boyish Wellness Update. Dorsum pain in the boyish. A convenient guide. second ed. 2005.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 22.7 Houghton K. Review for the generalist: evaluation of depression dorsum pain in children and adolescents. Pediatric Rheumatology. 2010;8(1):28.
- ↑ Kim H, Green D. Adolescent dorsum pain. Current Opinion in Pediatrics. 2008;20(1):37-45.
- ↑ Macias B, Murthy Grand, Chambers H, Hargens A. Asymmetric Loads and Pain Associated With Haversack Carrying past Children. Journal of Pediatric Orthopaedics. 2008;28(5):512-517.
- ↑ Rodriguez-Oviedo P, Ruano-Ravina A, Perez-Rios Chiliad, Garcia F, Gomez-Fernandez D, Fernandez-Alonso A et al. School children'due south backpacks, dorsum pain and dorsum pathologies. Archives of Affliction in Childhood. 2012;97(8):730-732.
- ↑ 26.0 26.1 Baker R, Patel D. Lower Dorsum Pain in the Athlete: Common Conditions and Treatment. Primary Care: Clinics in Role Exercise. 2005;32(1):201-229.
- ↑ COMBS J, CASKEY P. Dorsum Pain in Children and Adolescents. Southern Medical Journal. 1997;90(8):789-792.
- ↑ 28.0 28.1 Diepenmaat A. Cervix/Shoulder, Low Back, and Arm Pain in Relation to Computer Use, Physical Activeness, Stress, and Depression Among Dutch Adolescents. PEDIATRICS. 2006;117(ii):412-416.
- ↑ Standaert C. Spondylolysis: a disquisitional review. British Periodical of Sports Medicine. 2000;34(6):415-422.
- ↑ Kim H, Green D. Adolescent back pain. Electric current Stance in Pediatrics. 2008;20(ane):37-45.
- ↑ Micheli LJ, Woods, R. Dorsum pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995 Jan;149(1):xv-eight
- ↑ Orthoinfo.aaos.org. Adult Spondylolisthesis in the Depression Back-OrthoInfo - AAOS [Cyberspace]. 2015 [cited 15 Jan 2015]. Available from: http://orthoinfo.aaos.org/topic.cfm?topic=A00588
- ↑ Beutler West, Fredrickson B, Murtland A, Sweeney C, Grant W, Baker D. The Natural History of Spondylolysis and Spondylolisthesis. Spine. 2003;28(ten):1027-1035.
- ↑ Lonstein J. Spondylolisthesis in Children. Spine. 1999;24(24):2640.
- ↑ Motley Thou, Nyland J, Jacobs J, Caborn D. The Pars Interarticularis Stress Reaction, Spondylolysis, and Spondylolisthesis Progression. Periodical of Athletic Training. 1998;33:351-358.
- ↑ MORITA T, IKATA T, KATOH S, MIYAKE R. Lumbar Spondylolysis in children and Adolescents. Bone and Joint Surgery. 1995;77:620-625.
- ↑ SEITSALO S, STERMAN One thousand, HYVRINEN H, TALLROTH K, SCHLENZKA D, POUSSA M. Progression of Spondylolisthesis in Children and Adolescents. Spine. 1991;16(4):417-421.
- ↑ 0. Negrini South, Aulisa A, Aulisa L, Circo A, de Mauroy J, Durmala J et al. 2011 SOSORT guidelines: Orthopaedic and Rehabilitation handling of idiopathic scoliosis during growth. Scoliosis. 2012;7(one):3.
- ↑ 11. Altaf F, Gibson A, Dannawi Z, Noordeen H. Adolescent idiopathic scoliosis. BMJ. 2013;346(apr30 1):f2508-f2508.
- ↑ Miller N. CAUSE AND NATURAL HISTORY OF Adolescent IDIOPATHIC SCOLIOSIS. Orthopedic Clinics of North America. 1999;30(3):343-352.
- ↑ 13. OGILVIE J, SHERMAN J. Spondylolysis in Scheuermannʼs Disease. Spine. 1987;12(3):251-253.
- ↑ Lowe T. Scheuermann'south Kyphosis. Neurosurgery Clinics of Due north America. 2007;18(2):305-315.
- ↑ Micheli L. Back Pain in Young Athletes. Archives of Pediatrics; Adolescent Medicine. 1995;149(1):15.
- ↑ Frymoyer JW, Pope MH, Clements JH, Wilder DG, MacPherson B, Ashikaga T. Risk factors in low-dorsum hurting. An epidemiological survey. J Bone Joint Surg Am. 1983;65:213–218
- ↑ Kumar R, Kumar V, Das N, Behari S, Mahapatra A. Adolescent lumbar disc illness: findings and outcome. Childs Nerv Syst. 2007;23(eleven):1295-1299.
- ↑ Dang L, Liu Z. A review of current handling for lumbar disc herniation in children and adolescents. European Spine Journal. 2009;xix(2):205-214.
- ↑ xviii. Haidar R, Ghanem I, Saad S, Uthman I. Lumbar disc herniation in young children. Acta Paediatrica. 2009;.
- ↑ DePalma M, Bhargava A. Nonspondylolytic Etiologies of Lumbar Pain in the Young Athlete. Current Sports Medicine Reports. 2006;5(1):44-49.
- ↑ Spine-health. Potential Causes of Dorsum Pain in Children and Teens [Net]. 2015 [cited 14 January 2015]. Bachelor from: http://www.spine-health.com/weather condition/lower-back-pain/potential-causes-back-pain-children-and-teens
- ↑ Greenspan A, Jundt 1000, Remagen W, Greenspan A. Differential diagnosis in orthopaedic oncology. Philadelphia: Lippincott Williams & Wilkins; 2007.
- ↑ Cohen M, Harrington T, Ginsburg W. Osteoid osteoma: 95 cases and a review of the literature. Seminars in Arthritis and Rheumatism. 1983;12(3):265-281.
- ↑ Knott D. Ankylosing Spondylitis AS. Inflamed spine data. Patient | Patient.co.uk [Internet]. Patient.co.great britain. 2015 [cited 17 January 2015]. Available from: http://www.patient.co.great britain/doctor/ankylosing-spondylitis
- ↑ Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. Children. 2007 Dec one;100(five):10-one.
- ↑ Turner P, Green J, Galasko C. Back Pain in Childhood. Spine. 1989;14:812-814.
- ↑ Weinstein S. The Pediatric Spine: Principles and Practice. 2nd ed. Philadelphia: Lippincott, Williams and Wilkins; 2001.
- ↑ Bradford D, Hensinger R. The Paediatric Spine. New York: Thieme Publishing Group; 1985.
- ↑ Calvo-Muñoz I, Gómez-Conesa A, Sánchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatrics. 2013;13(1):fourteen.
- ↑ Smith D, Leggat P. Dorsum Pain in the Young: A Review of Studies Conducted Among School Children and University Students. CPR. 2007;three(one):69-77.
- ↑ 59.0 59.i 59.ii 59.3 59.4 59.five Auerbach J, Ahn J, Zgonis M, Reddy S, Ecker M, Flynn J. Streamlining the Evaluation of Depression Back Pain in Children. Clin Orthop Relat Res. 2008;466(viii):1971-1977.
- ↑ 60.0 threescore.ane threescore.2 Magee D. Orthopedic concrete cess. St. Louis, Mo.: Saunders Elsevier; 2006.
- ↑ 61.0 61.1 Chou R. Diagnosis and Handling of Depression Back Pain: A Joint Clinical Practice Guideline from the American Higher of Physicians and the American Pain Society. Register of Internal Medicine. 2007;147(7):478.
- ↑ Downie A, Williams C, Henschke N, Hancock One thousand, Ostelo R, de Vet H et al. Red flags to screen for malignancy and fracture in patients with low back pain: systematic review. BMJ. 2013;347(dec11 ane):f7095-f7095.
- ↑ Greenhalgh Southward, Selfe J. A qualitative investigation of Cerise Flags for serious spinal pathology. Physiotherapy. 2009;95(3):223-226.
- ↑ Jakes Advertisement, Phillips R, Scales M. Teenagers with back pain. Bmj. 2015 April two;350:h1275.
- ↑ Sjolie North. Psychosocial correlates of low-back pain in adolescents. European Spine Journal. 2002;11(six):582-588.
- ↑ Staes F, Stappaerts One thousand, Lesaffre E, Vertommen H. Depression dorsum pain in Flemish adolescents and the part of perceived social support and effect on the perception of back pain. Acta Paediatrica. 2003;92(4):444-451.
- ↑ 67.0 67.one Jones 1000, Watson K, Silman A, Symmons D, Macfarlane G. Predictors of Depression Dorsum Pain in British Schoolchildren: A Population-Based Prospective Cohort Written report. PEDIATRICS. 2003;111(4):822-828.
- ↑ Watson Yard, Papageorgiou A, Jones G, Taylor S, Symmons D, Silman A et al. Low dorsum pain in schoolchildren: the function of mechanical and psychosocial factors. Archives of Disease in Childhood. 2003;88(one):12-17.
- ↑ Kopec J, Sayre E. Stressful Experiences in Childhood and Chronic Back Hurting in the Full general Population. The Clinical Periodical of Hurting. 2005;21(half-dozen):478-483.
- ↑ Lynch A, Kashikar-Zuck Due south, Goldschneider K, Jones B. Psychosocial Risks for Disability in Children With Chronic Back Pain. The Periodical of Pain. 2006;7(iv):244-251.
- ↑ 71.0 71.1 Ralston S, Weir Thousand. Suspecting Lumbar Spondylolysis in Adolescent Low Dorsum Pain. Clinical Pediatrics. 1998;37(5):287-293.
- ↑ 72.0 72.one Roberts F, Kishore P, Cunningham Yard. Routine oblique radiography of the pediatric lumbar spine: is it necessary?. American Journal of Roentgenology. 1978;131(2):297-298.
- ↑ 73.0 73.1 73.2 Ryan P, Evans P, Gibson T, Fogelman I. Chronic low back pain: comparison of bone SPECT with radiography and CT. Radiology. 1992;182(3):849-854.
- ↑ 74.0 74.1 Cohen E, Stuecker R. Magnetic resonance imaging in diagnosis and follow-upwards of impending spondylolysis in children and adolescents: early treatment may prevent pars defects. Journal of Pediatric Orthopaedics B. 2005;14(2):63-67.
- ↑ 75.0 75.1 Feldman D, Hedden D, Wright J. The Use of Os Scan to Investigate Back Pain in Children and Adolescents. Journal of Pediatric Orthopaedics. 2000;twenty(6):790-795.
- ↑ 76.0 76.1 Goda Y, Sakai T, Sakamaki T, Takata Y, Higashino Thou, Sairyo K. Analysis of MRI bespeak changes in the adjacent pedicle of boyish patients with fresh lumbar spondylolysis. European Spine Journal. 2014;23(ix):1892-1895.
- ↑ 77.0 77.1 77.2 77.3 77.iv 77.5 77.6 77.vii Calvo-Muñoz I, Gómez-Conesa A, Sánchez-Meca J. Physical therapy treatments for low dorsum pain in children and adolescents: a meta-analysis. BMC Musculoskeletal Disorders. 2013;14(1):55. (LoE: 1A)
- ↑ Heymans Grand, van Tulder M, Esmail R, Bombardier C, Koes B. Back Schools for Nonspecific Low Dorsum Pain. Spine. 2005;30(xix):2153-2163. (LoE: 1A)
- ↑ Aure O, Hoel Nilsen J, Vasseljen O. Manual Therapy and Exercise Therapy in Patients With Chronic Depression Dorsum Pain. Spine. 2003;28(6):525-531. (LoE:1B)
- ↑ 80.0 lxxx.1 80.2 De Luigi A. Low Back Pain in the Adolescent Athlete. Concrete Medicine and Rehabilitation Clinics of North America. 2014;25(4):763-788. (LoE:A)
- ↑ 81.0 81.1 Michaleff Z, Kamper Due south, Maher C, Evans R, Broderick C, Henschke N. Low back pain in children and adolescents: a systematic review and meta-analysis evaluating the effectiveness of conservative interventions. European Spine Journal. 2014;23(10):2046-2058. (LoE:1A)
- ↑ Curtis C, d' Hemecourt P. Diagnosis and management of back pain in adolescents. Adolesc Med Country Art Rev. 2007 May;eighteen(1):140–64, ten. (LoE: 5)
- ↑ 83.0 83.1 83.2 Purcell L, Micheli L. Low Back Pain in Young Athletes. Sports Health: A Multidisciplinary Approach. 2009;one(3):212-222. (LoE:B)
- ↑ 84.0 84.1 Vidal J, Borràs P, Ponseti F, Cantallops J, Ortega F, Palou P. Furnishings of a postural instruction program on school backpack habits related to low back pain in children. European Spine Journal. 2012;22(4):782-787. (LoE: 1B)
- ↑ Ickmans Chiliad, Voogt L, Nijs J. Rehabilitation Succeeds Where Technology and Pharmacology Failed: Effective Treatment of Persistent Pain beyond the Lifespan.
- ↑ 86.0 86.1 Kordi R, Rostami One thousand. Low back hurting in children and adolescents: an algorithmic clinical approach. Iranian journal of pediatrics. 2011 Sep;21(iii):259.
- ↑ 87.0 87.1 Jones M, Stratton M, Reilly T, Unnithan Five. Recurrent non-specific depression-back pain in adolescents: the office of exercise. Ergonomics. 2007;50(10):1680-1688. (LoE: 1B)
- ↑ Cardon G, de Clercq D, Geldhof E, Verstraete Southward, de Bourdeaudhuij I. Back education in simple schoolchildren: the effects of adding a physical activity promotion program to a back care program. European Spine Periodical. 2006;16(ane):125-133. (LoE: 2B)
- ↑ Ahlqwist A, Hagman Thou, Kjellby-Wendt G, Beckung E. Physical Therapy Handling of Back Complaints on Children and Adolescents. Spine. 2008;33(20):E721-E727. (LoE: 1B)
- ↑ Fritz J, Clifford S. Depression Dorsum Pain in Adolescents: A Comparing of Clinical Outcomes in Sports Participants and Nonparticipants. Periodical of Athletic Training. 2010;45(1):61-66. (LoE: 3B)
Source: https://www.physio-pedia.com/Adolescent_Back_Pain
0 Response to "Risk Factors Low Back Pain Baker 2009 Systematic Review Sleeping Sport Sitting Walking"
Post a Comment